Year Ender 2022: Mpox, Tomato Flu, West Nile Fever — Diseases That Gripped The World
Diseases in 2022: Apart from Covid-19, mpox disease, Lassa fever, West Nile fever, Marburg virus disease, Zika, tomato flu, and camel flu were some of the diseases that gripped the world this year.

Diseases in 2022: The year 2022 saw the emergence of new viruses, outbreaks of some diseases, and cases of several infections. Apart from Covid-19, mpox disease (previously monkeypox), Lassa fever, West Nile fever, Marburg virus disease, Zika virus disease, tomato flu, camel flu, and Crimean-Congo Haemorrhagic fever were some of the diseases that gripped the world this year. Langya henipavirus and Khosta-2 are two viruses newly discovered in 2022.
In December, South Korea registered its first death from infection caused by Naegleria fowleri, commonly called the "brain-eating amoeba".
Here is the list of diseases, infections and viruses that were in the news in 2022.
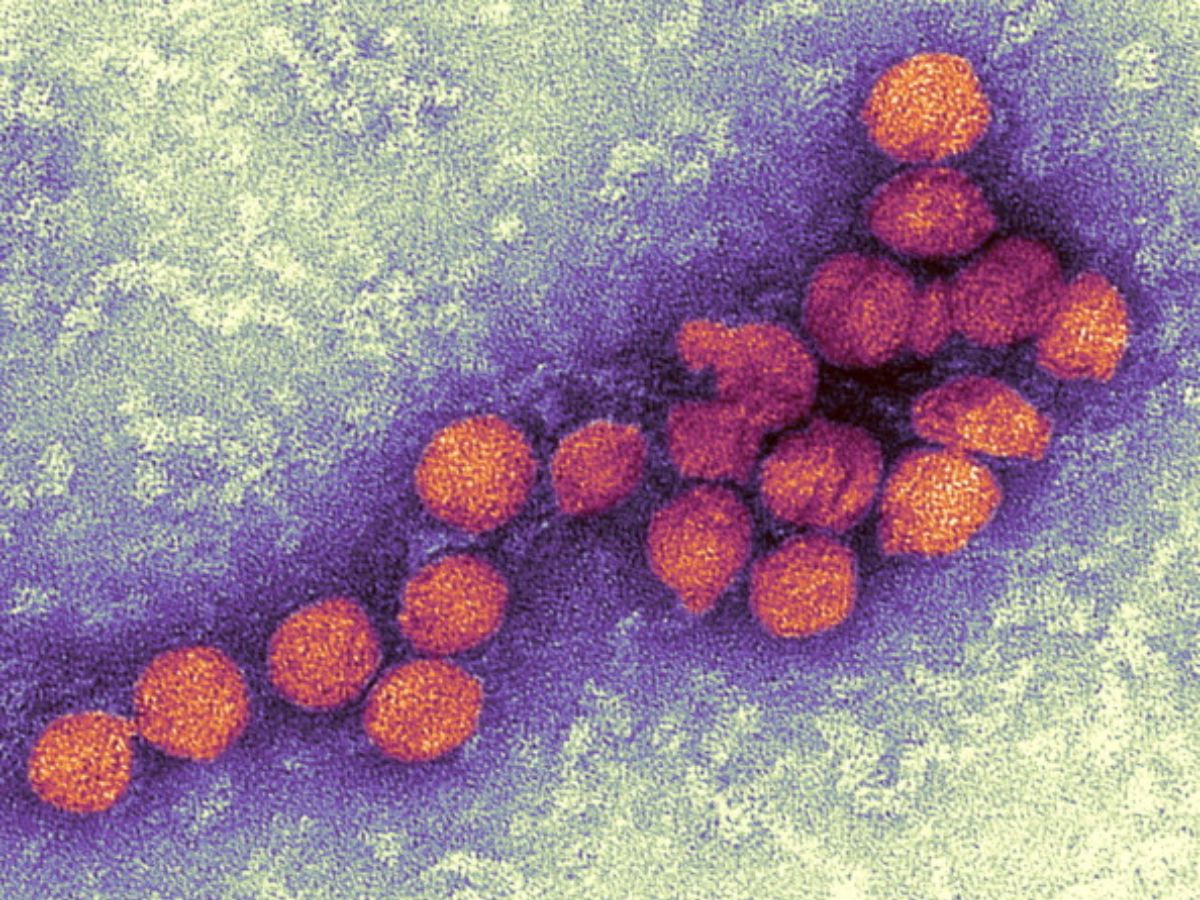
Mpox
On May 6, 2022, the first case of mpox, previously monkeypox, was detected in London. At that time, the person had a recent travel history from Nigeria, where mpox is endemic. However, on May 16, the UK Health Security Agency (UKHSA) confirmed four new cases of mpox in London with no travel history from a country where mpox is endemic.
On May 18, the first case of mpox was identified in the United States. The infection was found in an adult man from Massachusetts who had recently travelled to Canada. Since May 18, cases of mpox began to be reported from an increasing number of countries and regions, mostly in Europe and the Americas. Cases were also reported in Asia, Africa and Oceania. The 2022 mpox outbreak marks the first time the virus has spread widely outside Central and West Africa.
World Health Organization (WHO) chief Tedros Adhanom Ghebreyesus declared the mpox outbreak a public health emergency of international concern (PHIEC) on July 23.
ALSO READ | All You Need To Know About Mpox
On November 28, WHO recommended using the term 'mpox' instead of monkeypox, citing racist and stigmatising language online as the reason behind the change of name.
Mpox is a rare zoonotic disease (infectious disease that is transmitted between species from animals to humans or from humans to animals) caused by infection with mpox virus, and does not spread easily between people. Since mpox is a mild self-limiting illness, most people recover from the disease within a few weeks. However, some individuals can suffer from severe illness.
Though there is a very low risk of transmission to the general population, mpox can be spread when someone is in close contact with an infected person.
The mpox virus belongs to the Orthopoxvirus genus in the family Poxviridae, and was first discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research.
ALSO READ | Antivirals May Reduce Symptoms In Monkeypox Patients, Suggests Study In Lancet
The Orthopoxvirus genus includes variola virus, which causes smallpox, vaccinia virus, which is used in the smallpox vaccine, and cowpox virus.
In 1970, the first human case of mpox was recorded in the Democratic Republic of Congo (DRC), during a period of intensified effort to eliminate smallpox, according to the CDC. Since 1970, mpox has been reported in several other central and western African countries.
Mpox virus has emerged as the most important Orthopoxvirus, following the eradication of smallpox in 1980, according to the WHO. People outside of Africa have also suffered from mpox. Cases have been reported in the United States, Israel, Singapore, and the UK.
According to the CDC, the natural reservoir of mpox remains unknown. African rodents and non-human primates such as monkeys may harbour the mpox virus and infect people.
Mpox Symptoms
The symptoms of mpox in humans are similar to but milder than the symptoms of smallpox. The infection can be divided into two periods — the invasion period and the skin eruption period. The invasion period lasts between zero to five days.
The disease begins with fever, headache, muscle aches, back aches, swollen lymph nodes, chills, and exhaustion.
Smallpox and mpox are different in the fact that the latter causes lymph nodes to swell, while smallpox does not. The swelling of lymph nodes is called lymphadenopathy. The incubation period of mpox is usually seven to 14 days, but can range from five to 21 days, according to the CDC.
ALSO READ | EXPLAINED: Is Monkeypox A Sexually Transmitted Disease? Know What Experts Say
During the skin eruption period, the patient develops a rash within one to three days after the appearance of the fever. The rashes begin on the face, then spread to other parts of the body.
Lesions progress through the stages of macules, papules, vesicles, pustules, and scabs before falling off. Mpox typically lasts two to four weeks.
Is there any treatment for monkeypox?
There is currently no proven, safe treatment for mpox virus infection.
An mpox outbreak can be controlled with the help of smallpox vaccine, cidofovir, ST-246, and vaccinia immune globulin (VIG). Using the best available information about the benefits and risks of smallpox vaccination and drug use, CDC guidance was developed for the prevention and management of mpox and other orthopoxvirus infections.
According to the WHO, clinical care for mpox should be fully optimised to alleviate symptoms, manage complications, and prevent long-term sequelae, which is the consequence of a previous disease or injury. Adequate nutritional status can be maintained throughout consumption of fluids and healthy food.
ALSO READ | List Of Therapeutics And Vaccines Available For Mpox Treatment
Based on data in animal and human studies, an antiviral agent known as tecovirimat that was developed for smallpox was licensed by the European Medical Association (EMA) for mpox in 2022. However, tecovirimat is not yet widely available.
Though data is not available on the effectiveness of Cidofovir and Brincidofovir in treating human cases of mpox, both have proven capacity against poxviruses in vitro and animal studies.
Vaccination against smallpox was demonstrated through several observational studies to be about 85 per cent effective in preventing mpox, which means that prior smallpox vaccination may result in milder illness. Smallpox vaccines can protect people from getting mpox because the mpox virus is closely related to the virus causing smallpox.
Imvamune or Imvanex (JYNNEOS), is a vaccine that has been licensed in the United States to prevent mpox and smallpox.
A clinical study on the immunogenicity of JYNNEOS and efficacy data from animal studies have shown that JYNNEOS is effective against mpox.
Vaccination after an mpox exposure may help prevent the disease or make it less severe, according to experts.
ACAM2000, which contains a live vaccinia virus (closely related to the virus that causes cowpox), is licensed for Immunisation in people who are at least 18 years of age, and at high risk for smallpox infection, and can also be used in people exposed to mpox when administered under an expanded access investigational new drug protocol.
No data is available on the effectiveness of vaccinia immune globulin (VIG) in treatment of mpox complications. VIG has no proven benefit in the treatment of smallpox complications, and its use is administered as an Investigational New Drug (IND).
Whether a person with severe mpox infection will benefit from treatment with VIG is not known. However, the use of this vaccine may be considered in such instances.
Lassa Fever
In February 2022, three cases of Lassa fever were confirmed in the United Kingdom, one of whom died on February 11. This marked the first time cases of Lassa fever were reported in the UK since 2009.
The cases reported in the UK were within the same family in the east of England and linked to recent travel to West Africa.
Lassa fever is an animal-borne, or zoonotic, acute viral illness, that is endemic in parts of West Africa, according to the CDC, the national public health agency of the United States. The haemorrhagic illness is caused by the Lassa virus, which is a member of the virus family Arenaviridae, a single-stranded RNA virus.
Lassa fever was discovered in 1969 when two missionary nurses died in Nigeria. The first cases were confirmed in Lassa, a Nigerian town, and the virus is named after the town.
The animal vector for Lassa virus is Mastomys natalensis, the "multimammate rat".
Symptoms of Lassa fever
The signs and symptoms of Lassa fever are usually mild and typically occur one to three weeks after a person is infected. Most people infected with the disease have mild symptoms and hence, go undiagnosed. The mild symptoms include slight fever, general malaise, and weakness, and headache, according to the CDC.
The disease may progress to more serious symptoms including haemorrhaging in gums, eyes, or nose, respiratory distress, repeated vomiting, facial swelling, pain in the chest, back, and abdomen, and shock, in 20 per cent of infected individuals.
Hearing loss, tremors, and encephalitis are some of the neurological problems occurring due to Lassa fever.
ALSO READ | What Is Lassa Fever? Know Symptoms, Treatment
Within two weeks after symptom onset, death may occur due to multi-organ failure.
The most common complication of Lassa fever is deafness. In approximately one-third of infections, various degrees of deafness occur. Hearing loss is permanent in many cases.
Severity of disease does not affect this complication. This is because deafness may develop in mild as well as in severe cases.
Around 15 per cent to 20 per cent of patients hospitalised for Lassa fever die from the illness. Only one per cent of all Lassa virus infections result in death.
One in five infections results in severe disease, where organs such as the liver, spleen, and kidneys are affected.
For women in the third trimester of pregnancy, the death rates for women are particularly high. A serious complication of infection is spontaneous abortion, with an estimated 95 per cent mortality in foetuses of infected pregnant mothers.
Clinical diagnosis of Lassa fever is often difficult because the symptoms are so varied and non-specific. The disease is also associated with occasional epidemics, during which the case-fatality can reach as high as 50 per cent in hospitalised patients.
West Nile Fever
On May 29, a man in Thrissur, Kerala, died from West Nile Fever. Two of his bystanders were also found to be suffering from West Nile Fever.
West Nile Fever is a disease caused by the West Nile Virus, which is a flavivirus, and causes disease in humans, horses, and several species of birds. Flavivirus is a group of positive, single-strand RNA viruses which mostly have arthropod vectors, and cause a number of serious human diseases such as yellow fever, dengue, encephalitis, hepatitis C, and West Nile Fever. West Nile Virus is related to the viruses which cause St Louis encephalitis, Japanese encephalitis, and yellow fever.
Most of the people who are infected with West Nile Virus show signs of illness. However, only some of them develop severe neurological illness which can be fatal.
ALSO READ | What Is West Nile Fever?
West Nile Virus has an extremely broad host range, and replicates in birds, reptiles, amphibians, mammals, mosquitoes, and ticks, according to the World Organisation for Animal Health (OIE).
The reservoir of West Nile Virus is in birds. When mosquitoes bite an infected bird ingesting the virus in the blood, they act as carriers or vectors spreading the virus from the bird to other birds and animals. In this way, the virus circulates from bird to bird through mosquito bites, and is amplified at each cycle.
Mosquito species of the genus Culex are generally considered the principal vectors of West Nile Virus, particularly Culex pipiens. The virus is maintained in mosquito populations through vertical transmission, which is movement from adults to eggs.
Symptoms of West Nile Fever
About eight out of 10 people infected with West Nile Virus do not develop any symptoms.
Febrile illness or fever is seen in some people. About one in five people infected with West Nile Virus develop a fever with other symptoms such as headache, body aches, joint pains, vomiting, diarrhoea, or rash, according to the CDC. Though people with febrile illness due to West Nile Virus recover completely, fatigue and weakness can persist for weeks or months.
Marburg Virus Disease

On July 10, two people from West African country Ghana tested positive for the Marburg virus. The Ghana Health Service confirmed the cases on July 18.
The Marburg virus is a highly infectious disease similar to Ebola.
The Ghana Health Service confirmed the two cases after two persons who later died tested positive for the Marburg virus earlier in July. This was Ghana's first outbreak of Marburg virus disease.
Marburg virus disease was previously known as Marburg haemorrhagic fever. It is a severe illness in humans caused by the Marburg virus. The Marburg virus disease has a case fatality ratio of up to 88 per cent, but can be much lower with good patient care. The case fatality rate depends on the virus strain and case management.
Marburg virus disease can affect both people and non-human primates.
ALSO READ | Explained: What Is Marburg Virus Disease? All About The Illness
Both the Marburg and Ebola viruses are members of the Filoviridae family (filovirus), and cause diseases which are clinically similar. The Marburg virus is a genetically unique zoonotic RNA virus of the filovirus family.
Both Marburg virus disease and Ebola virus disease are rare. They can result in outbreaks with high fatality rates.
The reservoir host of Marburg virus is the African fruit bat, Rousettus aegyptiacus, which belongs to the Pteropodidae family.
According to the WHO, the Marburg virus is transmitted to humans from fruit bats and spreads among humans through human-to-human transmission.
Symptoms of Marburg Virus Disease
The incubation period of the Marburg virus, which is the interval from infection to onset of symptoms, varies from two to 21 days.
Illness resulting from Marburg virus infection begins abruptly, with high fever, malaise, severe headache, and muscle aches.
On the third day, abdominal pain, watery diarrhoea, nausea, cramping, and vomiting may occur. Moreover, diarrhoea can persist for a week.
At this phase, patients may have "ghost-like" drawn features, expressionless faces, deep-set eyes, and extreme lethargy, according to the WHO.
ALSO READ | Germany 1967 To Ghana 2022: History Of Marburg Virus Disease Outbreaks Reported Across The World
Non-itchy rash was a feature observed in most patients during the 1967 European outbreak, between two and seven days after the onset of symptoms.
Several patients develop severe haemorrhagic manifestations between five and seven days. Bleeding from multiple areas may occur in fatal cases. Sometimes, traces of fresh blood are found in the patients' vomit and faeces. There could also be bleeding from the nose, vagina, and gums. A maculopapular rash, most prominent in the trunk, which includes the chest, back, and stomach, may occur around the fifth day after the onset of symptoms. A macule is a flat, reddened area of skin present in a rash, while a papule is a raised area of skin in a rash. The term maculopapular is used to describe a rash with both flat and raised parts.
Sometimes, symptoms may become increasingly severe and can include jaundice, inflammation of the pancreas, severe weight loss, delirium, shock, liver failure, massive haemorrhaging, and multi-organ dysfunction.
Spontaneous bleeding may occur at venipuncture sites, which are the regions where intravenous access is obtained to give fluids or obtain blood samples.
Patients can have sustained high fevers during the severe phase of illness. If the central nervous system is affected, it can cause confusion, irritability, and aggression.
In the late phase of disease, which is after 15 days, orchitis or inflammation of one or both testicles has been reported occasionally.
Death may occur between eight and nine days after symptom onset, in fatal cases, and is usually preceded by severe blood loss and shock.
Tomato flu

In May 2022, a new virus known as tomato flu, or tomato fever, emerged in the state of Kerala in children younger than five years. Tomato flu was first identified in the Kollam district of Kerala, on May 6, 2022.
According to a report published in the journal The Lancet Respiratory Medicine, more than 82 cases of tomato flu in children below five years of age were reported by local government hospitals, as of July 26, 2022.
Tomato flu is a rare viral infection that could be a new variant of the viral hand-foot-and-mouth disease, a common infectious disease targeting mostly children aged one to five years and immunocompromised adults. In some case studies, hand-foot-and-mouth disease has been found in immunocompetent adults. Hand-foot-and-mouth disease is a mild, contagious viral infection common in young children, and causes symptoms such as sores in the mouth and rashes on the hands and feet.
ALSO READ | All You Need To Know About Tomato Flu
The symptoms of tomato flu are similar to those of Covid-19. Both tomato flu and Covid-19 are associated with symptoms such as fever, fatigue, and body aches. Some patients with Covid-19 report rashes on the skin.
However, the tomato flu virus is not related to SARS-CoV-2. Tomato flu is a self-limiting illness, which means that it tends to go away on its own, without treatment. According to the Lancet report, tomato flu is currently in an endemic state and is considered non-life threatening. However, vigilant management is desirable to prevent further outbreaks because of the unpleasant experience of the Covid-19 pandemic. There is no specific drug to treat tomato flu.
Symptoms of Tomato Flu
Tomato flu is a rare viral infection that could be a new variant of the viral hand-foot-and-mouth disease, a common infectious disease targeting mostly children aged one to five years and immunocompromised adults. In some case studies, hand-foot-and-mouth disease has been found in immunocompetent adults. Hand-foot-and-mouth disease is a mild, contagious viral infection common in young children, and causes symptoms such as sores in the mouth and rashes on the hands and feet.
The symptoms of tomato flu are similar to those of Covid-19. Both tomato flu and Covid-19 are associated with symptoms such as fever, fatigue, and body aches. Some patients with Covid-19 report rashes on the skin.
However, the tomato flu virus is not related to SARS-CoV-2. Tomato flu is a self-limiting illness, which means that it tends to go away on its own, without treatment. According to the Lancet report, tomato flu is currently in an endemic state and is considered non-life threatening. However, vigilant management is desirable to prevent further outbreaks because of the unpleasant experience of the Covid-19 pandemic. There is no specific drug to treat tomato flu.
Crimean-Congo haemorrhagic fever

Spain confirmed a case of Crimean-Congo haemorrhagic fever on July 21, 2022. The infected man was admitted to a local hospital in Leon because he started showing symptoms of Crimean-Congo haemorrhagic fever after being bitten by a tick.
In 2011, Spain detected its first case of Crimean-Congo haemorrhagic fever. A Spanish man was bitten by a tick in 2016, following which he was diagnosed with the disease, and subsequently died.
Crimean-Congo haemorrhagic fever (CCHF) is caused by infection with Nairovirus, a tick-borne virus belonging to the Bunyaviridae family. The disease was first detected in Crimea, a peninsula in Eastern Europe, in 1944. Therefore, it was initially named Crimean haemorrhagic fever. In 1969, the disease was recognised as the cause of illness in the Congo, following which it was named Crimean-Congo haemorrhagic fever.
ALSO READ | What Is Crimean-Congo Haemorrhagic Fever?
The Crimean-Congo haemorrhagic fever virus has a case fatality rate of 10 to 40 per cent, and results in severe viral haemorrhagic fever outbreaks.
The disease is endemic in the Middle East, the Balkans, Africa, and some countries in Asia. It is also found in Eastern Europe, northwestern China, southern Europe, and the Indian subcontinent.
Transmission of Crimean-Congo haemorrhagic fever
Different wild animals and domestic animals such as sheep, goats, and cattle may serve as the hosts of the Crimean-Congo haemorrhagic fever virus. While several birds are resistant to infection with the virus, ostriches are susceptible. In endemic areas, ostriches may show a high prevalence of infection, and spread the disease to humans. Earlier, an outbreak of Crimean-Congo haemorrhagic fever had occurred at an ostrich abattoir in South Africa.
When ticks infected with the Crimean-Congo haemorrhagic fever virus bite livestock animals, the latter get infected as well. After this, the virus remains in their bloodstream for about one week. This allows the tick-animal-tick cycle to continue when another tick bites, according to the WHO. The principal vector for the virus belongs to the genus Hyalomma, which includes hard-bodied ticks common in Asia, Europe, and North Africa.
The Crimean-Congo haemorrhagic fever virus is spread either by tick bites or through contact with infected animal blood or tissues during or immediately after slaughter, according to the WHO. Ticks which are both a reservoir and a vector for the Crimean-Congo haemorrhagic fever virus are called Ixodid ticks.
Symptoms of Crimean-Congo haemorrhagic fever
The mode of acquisition of the virus determines the length of the incubation period. It may take three to nine days for the symptoms to appear following infection by a tick bite. When a person is infected through contact with infected blood or tissues, the incubation period is usually five to six days, with a maximum of 13 days.
A person suffering from Crimean-Congo haemorrhagic fever can show symptoms such as fever, dizziness, myalgia, backache, neck pain, stiffness, sore eyes, headache, joint pain, and photophobia, which refers to sensitivity to light. Other symptoms include abdominal pain, vomiting, nausea, diarrhoea, sore throat, confusion, and sharp mood swings.
The agitation may be replaced by sleepiness and depression, about two to four days after the onset of symptoms. Abdominal pain in Crimean-Congo haemorrhagic fever patients usually occurs in the upper right quadrant. Hepatomegaly or liver enlargement may also occur.
Camel Flu

People who attended the FIFA World Cup 2022, held in Qatar, and also the players, were at risk of viral respiratory infections including Covid-19 and Middle East Respiratory Syndrome (MERS), also known as camel flu.
MERS-CoV, a coronavirus that causes camel flu, had resulted in multiple hospital outbreaks in Saudi Arabia, but a limited number of cases in Qatar.
People at greater risk of developing MERS must avoid contact with dromedary (one-humped) camels, should not eat meat that has not been cooked properly, and must not drink raw camel milk or camel urine.
What is MERS?
MERS is a respiratory infection caused by the virus Middle East respiratory syndrome coronavirus (MERS-CoV), which was identified for the first time in 2012.
Severe acute respiratory syndrome coronavirus-2, or the novel coronavirus, which causes Covid-19, is also a type of coronavirus. MERS mostly results in symptoms such as shortness of breath, fever and cough. Other symptoms include pneumonia, and gastrointestinal problems such as diarrhoea.
ALSO READ | Explained: What Is Camel Flu (MERS)?
Of every 10 patients with MERS, three or four have died, according to the CDC. About 35 per cent of MERS cases reported to the WHO have succumbed to the disease.
MERS-CoV is a zoonotic virus, which means that its transmission occurs between animals and people. Several Member States in the Middle East, Africa and South Asia have reported the incidence of MERS cases and linked the infections to dromedary camels.
The number of cases of human-to-human transmission of MERS outside healthcare settings is limited.
According to the CDC, health officials first reported MERS in Saudi Arabia in September 2012, but subsequent investigations identified that the first known cases of the disease occurred in Jordan, a Middle-Eastern country, in 2012.
All cases of MERS that have occurred so far have been linked through travel to, or residence in countries in and near the Arabian Peninsula. In 2015, the Republic of Korea experienced an outbreak of MERS. This marked the largest known outbreak of camel flu outside the Arabian Peninsula. A traveller returning from the Arabian Peninsula is believed to have initiated the outbreak.
People ranging from age one to 99 years can contract MERS.
Zika virus disease

On Monday, December 12, a five-year-old girl from Raichur, Karnataka, became the first confirmed case of Zika virus in the state. Karnataka Health Minister K Sudhakar said there is no need to worry or concern, because the state government is taking all the necessary measures, according to media reports.
Zika virus spreads mostly by the bite of infected Aedes mosquito species such as Aedes aegypti and Aedes albopictus. The virus can be transmitted from a pregnant woman to her foetus, and may result in birth defects. It may also be transmitted sexually.
First discovered in 1947, Zika virus is named after the Zika Forest in Uganda. The virus was detected in a Rhesus macaque monkey. The first human cases of Zika were detected in 1952. In the 1950s, cases of Zika virus disease were reported in African countries.
Since then, outbreaks of Zika virus disease have been reported in tropical Africa, Southeast Asia, and the Pacific Islands, according to the CDC.
ALSO READ | All About Zika Virus Disease
Sporadic human infections were detected across Africa and Asia, from the 1960s to 1980s.
Zika virus disease symptoms
The symptoms of Zika are similar to those of many other diseases, and hence, many cases may not have been documented.
The Zika virus infection outbreaks that occurred over the last decade were found to be associated with increased incidence of Guillain-Barré syndrome, according to the WHO. Guillain-Barré syndrome is a condition in which the immune system attacks the nerves, and is triggered by an acute bacterial or viral infection. Symptoms of this disease include weakness and tingling in the feet and legs that may spread to the upper body.
Zika virus disease was found to be associated with microcephaly, when the virus emerged in the Americas. Microcephaly is a condition in which a baby's head is significantly smaller than expected, often due to abnormal brain development, and occurs because of infections, malnutrition or exposure to toxins. In 2015, a large epidemic of Zika virus disease occurred in Brazil.
The WHO declared a Public Health Emergency of International Concern (PHIEC) regarding microcephaly, other neurological disorders and Zika virus, from February to November 2016. Soon, the causal link between Zika virus and congenital malformations was confirmed.
Aedes aegypti mosquitoes were responsible for Zika virus disease outbreaks throughout most of the Americas and in other regions. The same mosquito transmits diseases like dengue, chikungunya and yellow fever.
Travellers from active transmission areas are often found to be infected with the Zika virus disease.
From 2017 onwards, cases of Zika virus disease globally declined. In the Americas and other endemic regions, Zika virus transmission persists at low levels. In 2019, the first local mosquito-transmitted Zika virus disease cases were reported in Europe.
In 2021, Zika virus outbreak activity was detected in India. A total of 89 countries and territories have reported evidence of mosquito-transmitted Zika virus infection so far.
Langya henipavirus
China confirmed about 35 cases of the Langya henipavirus, a zoonotic virus newly discovered in the nation, in August this year.
A study titled 'A Zoonotic Henipavirus in Febrile Patients in China', published in the New England Journal of Medicine (NEJM), states that the Langya henipavirus was identified in a throat swab sample from one patient in eastern China. Febrile is an adjective used to describe someone showing symptoms of a fever. The Langya henipavirus was discovered during a surveillance of febrile patients with a recent history of animal exposure in eastern China.
The Langya henipavirus is a "phylogenetically distinct henipavirus" and has a genome organisation identical to that of other henipaviruses, according to the NEJM study.
The genome of Langya henipavirus is composed of 18,402 nucleotides. The virus is phylogenetically related to Mojiang henipavirus, which was discovered in southern China.
Symptoms of Langya henipavirus
According to the study, all the patients were presented with fever. Meanwhile, 54 per cent of the patients experienced fatigue, 50 per cent had cough, 50 per cent experienced anorexia, 46 per cent suffered from myalgia (pain in the muscles), 38 per cent had nausea, 35 per cent had suffered from headache, and 35 per cent experienced vomiting.
Other abnormalities observed in the patients included thrombocytopenia (deficiency of platelets in blood), leukopenia (low level of white blood cells in blood), and impaired liver and kidney function.
ALSO READ | Explained: What Is Langya Henipavirus? All About The Zoonotic Virus Outbreak Confirmed In China
Thrombocytopenia, leukopenia, impaired liver function, and impaired kidney function were observed in 35 per cent, 54 per cent, 35 per cent, and eight per cent of the patients, respectively.
Therefore, the study found that the common symptoms associated with Langya henipavirus are fever, fatigue, cough, anorexia, myalgia, nausea, headache, and vomiting.
Langya henipavirus was the only potential pathogen detected in 26 of the 35 patients with acute Langya henipavirus infection.
The study states that shrews may be a natural reservoir of Langya henipavirus.
Khosta-2 virus

As the world continues to battle Covid-19, a new virus similar to the novel coronavirus has emerged. The virus, called Khosta-2, was detected in Russian horseshoe bats in September 2022. Khosta-2 is a sarbecovirus, a type of respiratory virus. The majority of animal sarbecoviruses are only distantly related to known human pathogens and do not infect human cells. Severe acute respiratory syndrome coronavirus 1 (SARS-CoV-1) and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) are examples of sarbecoviruses.
ALSO READ | Explained: What Is Khosta-2? All About The New COVID Vaccine-Resistant Virus Detected In Russian Bats
Khosta-2 is a sarbecovirus discovered in Russia, and has been found to interact with ACE2 receptors, the same entry receptor as SARS-CoV-2.
Check out below Health Tools-
Calculate Your Body Mass Index ( BMI )
Calculate The Age Through Age Calculator
Related Video
Southern Rising Summit 2024: How Important is Self-Awareness? Insights from Anu Aacharya | ABP LIVE